Sleep Disordered Breathing
Sleep disordered breathing is a term used to described breathing difficulties during sleep. Sleep disorders are more common than you may realise but they can have detrimental effects on you AND your partner’s general and dental health. Most people aren’t aware that they have one but:
-
30% of people snore
-
9% of women, 25% men and 2-3% children have obstructive sleep apnoea (OSA)
-
20% of peoplebrux during the night (grind their teeth)
Snoring is often regarded as being ‘normal’ and is sometimes laughed about. There are often misconceptions too when it comes to snoring and OSA. People think it’s normal – it may be ‘normal’ for them but it’s not healthy. Also, ‘going to sleep quickly at night and sleeping for 10 hours’ is not necessarily a sign of a good night’s sleep – you may just be really exhausted by the time your head hits the pillow at night and quantity doesn’t equal quality when it comes to sleep.
Snoring can be benign and may be more of a disruption to the partner’s sleep than the snorer but snoring can lead to:
-
increased episodes of acid reflux,
-
enlarged uvula (dangly thing at the back of your throat)
-
there are some thoughts that the fluttering of the uvula/soft palate near/on the internal carotid artery increases chance of carotid atherosclerosis which can lead to a stroke
-
could be a sign of OSA
All children who snore or breathe loudly most nights of the week should be assessed. Other signs that a child may have sleep disordered breathing:
-
teeth grinding
-
laboured breathing
-
chronic behavioural problem – hyperactive, limited concentration
-
chronically tired, hard to wake in the morning
-
mouth breathers
-
bed wetting
-
excessive sweating and/or restless sleeping
-
gasp, choke or pause in breathing, have a lot of bad dreams/sleep walk
-
dark circles under the eyes
-
overweight/underweight
It is important to note that there can be permanent changes to children’s health/IQ if the sleep disorder is not identified and treated early enough (the younger the better).
Bruxism (grinding of teeth) is a behaviour that is still not 100% understood, however, more research is being done into this common behaviour that occurs more often during non-REM sleep. Those people who grind their teeth, seem to have a poorer quality of sleep. There seems to be a shift from blaming the grinding habit for causing micro arousals during sleep, to looking at whether micro arousals caused by sleep disordered breathing (reduced air flow) is actually the cause of grinding. In children, it is believed that in 80% of cases where children grind their teeth at night, their habit stops after they have their tonsils/adenoids removed. There is some thought that the action of teeth grinding may be an attempt to open up the airways.
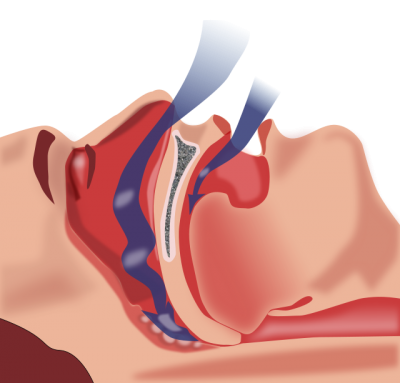
Obstructive sleep apnoea (OSA) is caused by an obstruction of the upper airway. It is characterised by repetitive pauses in breathing during sleep, despite the effort to breathe, and is usually associated with a reduction in blood oxygen saturation.
Signs of OSA:
-
dry mouth or sore throat in morning
-
reflux
-
fatigue, having to have day naps, falling asleep during the day easily
-
gasps for air during sleep, chokes, coughs
-
nightmares
-
frequent urination during the night
Some consequences of having poor quality sleep (adults and children):
-
alteration in mood and behaviour – depression, anxiety, irritability, ADHD in children
-
headaches in morning, teeth grinding
-
increased risk of hypertension
-
weight gain (less leptin and ghrelin hormones being released), difficulty losing weight
-
increased risk of congestive heart failure
-
growth and development delay, academic delay
-
poor concentration, foggy brain, memory
-
reduced reaction time, manual dexterity
-
reduced attention and vigilance
How is OSA treated?
There are various treatment options when it comes to OSA but your medical professional will usually recommend, for adults particularly, that a sleep study to be conducted. This can be conducted in a sleep clinic or in your own home. A diagnosis is then made by the sleep or respiratory specialist and your treatment options are discussed.
There are various treatment options for OSA and the success rate varies from person to person. These include:.
-
CPAP machines are the gold standard (moderate – severe apnoea) and work well but the compliance can sometimes be an issue even though the machines and nasal/mouth pieces have improved in comfort over the years.
-
Oral appliances are often recommended for mild-moderate apnoea and sometimes combined with a CPAP machine for more severe cases. There are numerous designs and can be tailored to your needs and budget. The appliances aim to reposition your bottom jaw forward and therefore open up the airway space at the back of your throat. These are tolerated quite well.
-
Oral myofunctional therapy, has been shown to reduce apnoeic episodes by 50% in adults and 63% in children (click on button below for 2014 Systematic Review and Meta-analysis on Myofunctional Therapy to treat OSA). This can be offered as an adjunct to the other treatment options – with oral appliance or CPAP machine.

-
Addressing weight-loss, allergies (rhinitis), alcohol intake, sleeping pills, smoking and sleep hygiene/behaviours. Sometimes correcting the sleep position (ie side sleeping) can improve the OSA. The consumption of alcohol does not allow for a good night’s sleep, especially in the later hours of the night, regardless of the presence of OSA
-
Tongue appliances suction your tongue forward and opening up the airway space if you have a large tongue. Nasal strips also are an inexpensive option, which are worn across the nose to widen the nasal passage. You can also purchase nasal plugs – which are worn in the nose opening and help those patients who may simply have nasal opening collapse. We can order you some of these devices, or you can order them yourself online.
-
Taping of the lips (micropore tape – from chemist) or wearing of a chin strap helps to keep the lips together at night and encourages nasal breathing which can help with snoring for some people.
-
Surgery to the soft palate and base of tongue is not recommended as often now due to limited long-term benefits but used to be done more routinely 10-20 years ago.
Please contact us if you have any questions regarding this information or if you are concerned about your or a family member’s sleep patterns. You never realise how poorly you feel until you actually get a good night’s sleep!!


